Dr. Kristina M. Deligiannidis has been the principal investigator on national multi-site clinical trials that led to the oral neuroactive steroid zuranolone’s approval
In a landmark decision, the U.S. Food and Drug Administration (FDA) has approved the first at-home oral pill, zuranolone, which will be sold under the brand named Zurzuvae, for treating perinatal or postpartum depression (PPD) – a condition one in eight birthing women experience. The decision is the culmination of decades of preclinical research done by scientists worldwide and the most recent clinical trials, led by Northwell Health’s The Feinstein Institutes for Medical Research’s Kristina M. Deligiannidis, MD, professor at the Institute of Behavioral Science at the Feinstein Institutes and the director of women’s behavioral health at Northwell’s Zucker Hillside Hospital.
This press release features multimedia. View the full release here: https://www.businesswire.com/news/home/20230807136425/en/
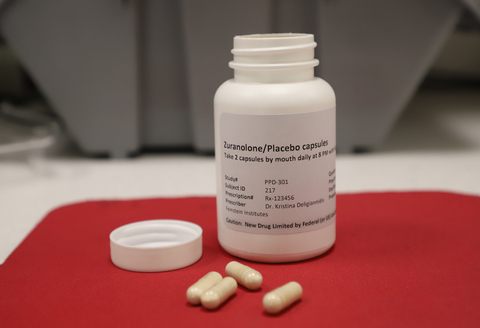
The national clinical trials for zuranolone were led by the Feinstein Institutes for Medical Research at Northwell Health. (Credit: Feinstein Institutes)
The announcement was made just days after findings from the SKYLARK Study, a phase 3 placebo-controlled clinical trial of zuranolone (50mg), was published in The American Journal of Psychiatry. Results showed rapid, clinically meaningful improvements in depressive symptoms. Some women reported a significant improvement in their symptoms by day three (after two doses) and sustained through day 45 (end of the trial).
“After years of dedicated research and collaboration with other scientists, women living with postpartum depression have a new, at-home, 14-day treatment option that has the potential to alleviate their symptoms,” said Dr. Deligiannidis. “PPD is often underdiagnosed and undertreated. With the FDA’s decision today, we may be able to reverse this and help many more women in need.”
Evidence suggests that PPD is partly due to a disruption in the normal interaction between the nervous system’s stress response, ɣ-aminobutyric acid (GABA) signaling and neuroactive steroids (NAS). The SKYLARK and ROBIN clinical trials – which provided the research data to support the FDA’s decisions – showed substantial results for improving depressive symptoms in women with PPD.
In 2021, Dr. Deligiannidis reported the publication of the phase 3 results of the ROBIN Study, which were published in the Journal of the American Medical Association (JAMA) Psychiatry. The trial demonstrated the improvement in depressive symptoms with zuranolone at 30 mg versus placebo in patients with PPD and that zuranolone was generally well tolerated. Based on those results, the team studied the safety and efficacy of 50 mg of zuranolone.
Over the past 15 years, Dr. Deligiannidis has received research support by the National Institutes of Health (NIH) and non-profit foundations to understand how neuroactive steroids are involved in the development of perinatal depression, specifically how they shape brain chemistry and brain circuitry in perinatal women. In 2019, through Dr. Deligiannidis’ clinical trial leadership, the FDA approved an intravenous infusion of the drug brexanolone (Zulresso) to treat the symptoms of PPD. While a landmark decision, the need for women to receive brexanolone at an infusion clinic or health system was a barrier to care. This new treatment, zuranolone, a pill, can be taken at home.
“Dr. Deligiannidis is a leader in clinical trials for postpartum depression, a condition that affects millions,” said Kevin J. Tracey, MD, president and CEO of the Feinstein Institutes, Karches Family Distinguished Chair in Medical Research. “The FDA approval stemming from her work will make available new therapeutic options that are clearly needed.”
The Feinstein Institutes and Dr. Deligiannidis lead in researching new methods to diagnose and treat perinatal depression. Recently she received more than $4 million in multi-year grants to use non-invasive brain imaging to study how the condition develops in women and to develop novel treatments, including bright light therapy, sleep modification and non-invasive vagus nerve stimulation to treat major depressive disorders.
About the Feinstein Institutes
The Feinstein Institutes for Medical Research is the research arm of Northwell Health, the largest health care provider and private employer in New York State. Home to 50 research labs, 3,000 clinical research studies and 5,000 researchers and staff, the Feinstein Institutes raises the standard of medical innovation through its five institutes of behavioral science, bioelectronic medicine, cancer, health innovations and outcomes, and molecular medicine. We make breakthroughs in genetics, oncology, brain research, mental health, autoimmunity, and are the global scientific leader in bioelectronic medicine – a new field of science that has the potential to revolutionize medicine. For more information about how we produce knowledge to cure disease, visit http://feinstein.northwell.edu and follow us on LinkedIn.
View source version on businesswire.com: https://www.businesswire.com/news/home/20230807136425/en/
Contacts
Matthew Libassi
631-793-5325
mlibassi@northwell.edu
